
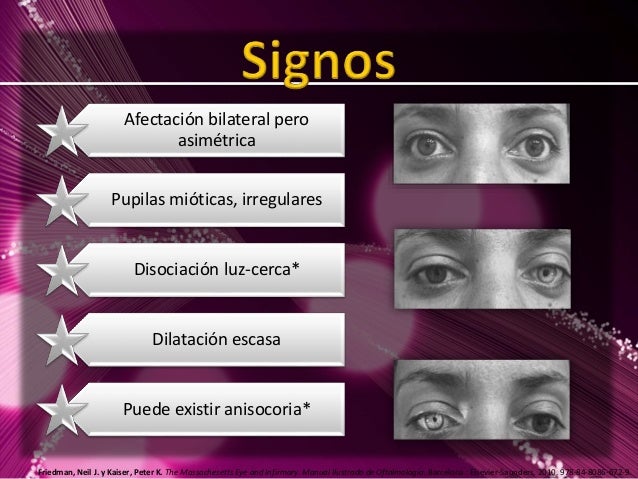
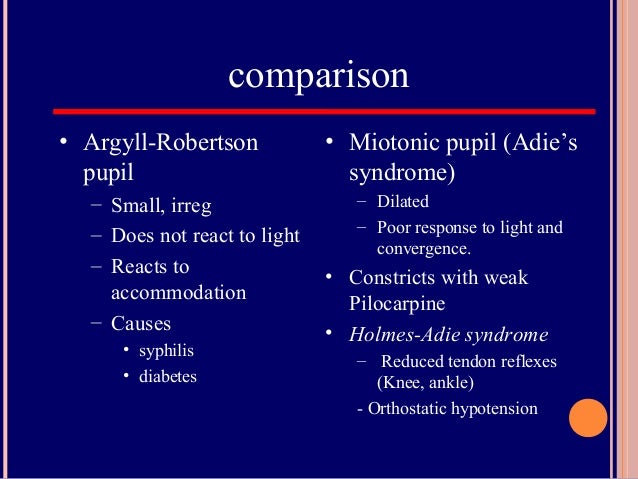
Medical: Manage co-existing heart failure, manage underlying cause (e.g.: antibiotics for infective endocarditis, penicillin for syphilis).Imaging: Chest radiograph (pulmonary oedema, pleural effusions, kerley B lines), echocardiogram (left ventricular function, valve anatomy, aortic root size, vegetatios).Bloods: FBC (anaemia, inflammatory markers), CRP/ESR (raised in infective endocarditis), treponemal tests (specific like EIA or TPHA, and non-specific like the VDRL and RPR).Bedside tests: Blood pressure (looking for a wide pulse pressure) and ECG (conduction blocks, LVH criteria), and then for features of infective endocarditis with temperature, urine dipstick (haematuria, proteinuria), and fundoscopy (Roth spots, Becker’s sign of retinal pulsations).If acute, think of dissection, infective endocarditis and prosthetic valve failure. Connective tissue disorders: Marfans, ehlers danlos, psuedoxanthoma elasticum, osteogenesis imperfecta.Rheumatological: HLA B27 associated arthopathies like ankylosing spondylitis.Infective: Infective endocarditis, rheumatic fever, tertiary syphilis.Degenerative: Bicuspid valves, age and factors like hypertension.The differential for an underlying cause of aortic regurgitation is: There is a similar murmur in pulmonary regurgitation either as a primary phenomenon or as a Graham Steell murmur secondary to pulmonary hypertension. The latter would not radiate and gives a “to-and-fro” quality to the sound. If this is the case you will need to decide which is the predominant lesions and bear in mind that even if the absence of a stenotic valve you can get a flow murmur across the aortic valve in the presence of regurgitant valves. Mixed valve disease: Listen for an accompanying ESM radiating to the carotids of aortic sclerosis.Syphilis: Argyll robertson pupil (small, irregular, depigmentation of the iris, accommodates but does not react to light).Infective endocarditis: Splinter haemorrhages, clubbing, leukonychia, oslers nodes, janeway lesions, pale palmar creases, conjunctival pallor, long lines for antibiotics, fever, evidence of previous surgery.If found, tell the examiner that you would like to enquire about features of inflammatory joint pain and uveitis, auscultate the lung apices for fibrosis and dipstick the urine for proteinuria of amyloidosis. Ankylosing spondylitis: Exaggerated thoracic kyphosis and loss of lumbar lordosis with compensatory extension of the neck and limited neck movements.
#ARGYLL ROBERTSON PUPIL VIDEO SKIN#
Connective tissue disorders: Marfan’s (tall, arachnodactyly, hypermobility, high arched palate), ehlers danlos (hypermobility, hyperextensible skin, fish mouth scars), psuedoxanthoma elasticum (plucked chicken skin appearance at the neck, axillae and antecubital fossae), osteogenesis imperfecta (blue sclerae though these can be seen in the other three conditions as well, bony deformities from prior poor healing of fractures).If you are confident about the diagnosis and wish to elicit further features, proceed to check for Durozier’s sign (systolic murmur over femorals with proximal compression and diastolic murmur with distal compression) and Traube’s sign (pistol-shot femorals with systolic and diastolic sounds). Check for additional features including heart failure (raised jugular venous pressure, 3rd heart sound, bi-basal crepitations, peripheral oedema) and infective endocarditis (see below). Auscultate for an early diastolic murmur heard loudest at the lower left sternal edge in expiration.
Looking at the neck, asses for prominent carotid pulsations suggestive of Corrigan’s sign. Inspect inside the mouth for the pulsating uvula of Muller’s sign, and check if the head is bobbing as part of De Musset’s sign. Look at the hands for Quincke’s sign and asses for a collapsing pulse. Scenarios: Shortness of breath, angina, syncope, dyspnoea.Įxamination of aortic regurgitation: On general inspection take note of any features that indicate an underlying connective tissue disorder or rheumatological disease. Hereditary Haemorrhagic Telangiectasia (HHT).Fascioscapulohumeral Muscular Dystrophy.



 0 kommentar(er)
0 kommentar(er)
